UNDERSTANDING PTSD (Pt. 2): Mythology
Jill Stoddard
by Lucas Myers 08/16/2013
Last week I shared a little bit about my experience working with San Diego’s veterans at Stand Down. This week I will address the questions and misconceptions that come up for many people in any conversation about Post-Traumatic Stress Disorder.
It has had many names, some going back as far as the American Civil War: shell shock, combat fatigue, soldier’s heart, combat neurosis, and, most recently, Post Traumatic Stress Disorder (PTSD). Some experts predict that as many as 30% of Iraq and Afghanistan combat veterans will receive treatment for PTSD. What was first observed as changes in soldiers that had survived combat is now recognized in many people who have witnessed, experienced, or even been affected by any of a variety of traumatic experiences.
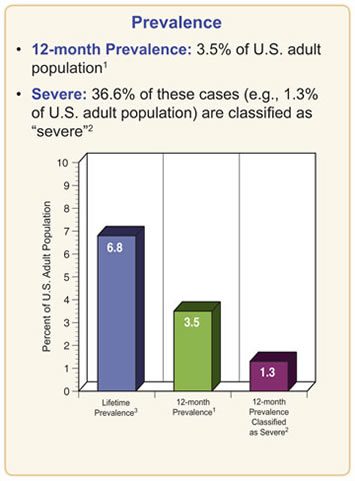
It is becoming increasingly common, affecting as many as 3.5 out of every 100 US residents according to the National Institute of Mental Health. Symptoms may include nightmares, flashbacks, uncontrollable thoughts about the traumatic event and severe anxiety. These experiences, along with very disruptive physiological effects related to anxiety, can persist for weeks, months, or years.
Most Americans are familiar with PTSD; it has been featured in major motion pictures from The Deer Hunter to Forrest Gump. Unfortunately, as with many complex subjects that receive the pop-culture treatment, PTSD is sometimes portrayed in a confusing and even irresponsible manner. Because of the widespread misunderstanding about PTSD and veterans who have been through combat, this week we will take a moment to address a few myths you may have heard.
MYTH: Everyone has been through a frightening experience that resulted in symptoms like PTSD. Eventually people get over it.
Fact: Frightening experiences may create vivid memories, however most people do not suffer the impairment and severity of symptoms characteristic of PTSD. Although there are many similarities between PTSD and other forms of anxiety, PTSD is unique in its effects on the brain's responses to events. PTSD can sometimes cause serious disability. It is a medical disorder than sometimes becomes complicated by co-occurring anxiety, mood, and substance-abuse disorders. It may cause significant problems in social interactions, relationships and ability to work.
MYTH: PTSD is a sign of “weakness” and “lack of character” in people who are unable to cope with difficult situations in the same way most people do.
Fact: For many people who have been exposed to markedly abnormal situations PTSD is a normal reaction. A person experiencing a traumatic event undergoes chemical changes in the brain in order to survive and function through his or her experience and these create symptoms that we recognize as PTSD. PTSD is not a result of moral failing or a weak character. Some studies suggest that half of all Americans will meet the criteria for a mental health diagnosis at some time in their lives.
MYTH: PTSD causes people to become violent and unpredictable.
Fact: Many people believe that mental health problems are associated with violence and unpredictability but this is rarely true. Someone with PTSD or another psychological condition should not be viewed as dangerous in the home or workplace. These fears result in stigmatizing diagnosis and treatment for people that need and deserve our respect, acceptance and help. PTSD and other psychological conditions only very rarely result in acts of aggression.
MYTH: Once you've been diagnosed with PTSD you will never recover. Therapy is a waste of time.
Fact: New studies are emerging all the time that show that most people with PTSD and other mental illnesses do get better and make full recoveries. Recovery may mean reduced symptoms and or the ability to lead a productive and fulfilling life. Many people recover their ability to live, work, learn, and participate in their communities. Some combination of therapy and medication plays a role in many recoveries and science has shown that hope and positive social support are two of the most important factors in predicting success.
MYTH: People with PTSD can't handle the everyday stress of finding and keeping a job.
Fact: If jobs weren't difficult and stressful we wouldn't pay people to do them. As with any other psychological condition, the severity of PTSD and an individual's path to recovery can vary widely. Balancing stress and stress tolerance well by matching employees’ needs to their work conditions leads to productivity and success. Studies show that most people with PTSD and other mental illnesses demonstrate motivation, punctuality, quality work, high attendance, and job tenure. Any employer can improve their gauge of workload and performance by considering these factors.
If you or someone you care about is struggling with PTSD or heightened anxiety as a result of serving in combat or another traumatic experience, and would like to speak with a professional at The Center for Stress and Anxiety Management, you may contact us at 858-354-4077 or csamsandiego@gmail.com
References:
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth
Edition. Arlington, VA, American Psychiatric Association, 2013. Web. [access date: 1 June
2013]. dsm.psychiatryonline.org
http://www.americasheroesatwork.gov/
http://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd/index.shtml
Reno, J. “Nearly 30% of vets treated by BA have PTSD”. Retrieved on August 18, 2003:
http://www.thedailybeast.com/articles/2012/10/21/nearly-30-of-vets-treated-by-v-a-have-ptsd.html
Tags: anxiety, PTSD, therapy, mental health treatment, San Diego, veterans, military, heroes, support