The following article was originally published in the OCD Newsletter in 1991. Back then, behaviorists were still telling people with the Pure-O form of OCD (where the sufferer experiences obsessions only), that they hoped medication would be of some benefit. To their knowledge, there were no known methods of treatment that reliably produced positive outcomes with this form of OCD. In 1987, I had developed a highly structured and formalized behavioral method of treating this form of OCD. These treatment guidelines were derived from current strategies, proposed by Dr. Edna Foa, for the treatment of the more traditional forms of OCD (e.g. contamination and checking). Specifically, the strategy called Exposure and Response Prevention (E&RP), entails the practice of having the patient voluntarily come in contact with the feared items or situations, and then manage the pursuant anxiety while not performing the undoing response. The adaptation of E&RP for the Pure-O required a few modifications, but essentially retained the same empirically-based treatment model. Initially, the duration of treatment for the Pure-O was significantly longer (two years), than the duration of the traditional treatment of OCD (six months to one year). Using the adaptation model of treating the Pure-O form, the success rate was achieved well into the 70% to 90% range. This was comparable to Dr. Foa’s findings. In the mid-1990’s, Mark Frearston, Ph.D. published one of the first controlled studies for the treatment of the Pure-O, using very similar methods to those proposed by my 1991 article. His methodology relied on a much stronger cognitive component than my approach, which, as discussed below, have retained a much stronger behavioral component. Cognitive treatment for anxiety disorders relies on helping people identify the irrational nature of their fears and find the evidence of their irrationality. My work with thousands of patients has lent strong support to the idea that the cognitive element is not nearly as important as the more strict behavioral element, which focuses on providing effective strategies for managing the threatening ideas, rather than debunking the specific irrationality of the idea. At this point (2004), I am finding that, with some slight innovations that I have laid out below, there are no differences in the treatment duration (approximately six to twelve months) for people with Pure-O and those with the compulsions of the more traditional form of OCD.
In my conceptualization of Obsessive-Compulsive Disorder, the tree of the overall syndrome has three main branches: the "obsessive-compulsive," the "responsibility O-C," and the purely obsessional thinker ("Pure-O"). In “Pure-O”, the anxiety emerges in response to an unwanted, intrusive thought or question; what I call a "spike." The ritual or compulsion with this form of OCD involves the non-observable, mental ‘pushing away’ of the thought, avoiding the recurrence of the thought, or attempting to solve the question or undo the threat that the thought presents. It should be remembered that most people who come into therapy tend to have a combination of these three distinct forms of OCD. Successfully treating one form typically has minimal effect on the others. When persons present with more than one form of OCD, treatment will tend to initially focus on the observable rituals, since they are generally easier to treat and provide a positive momentum for further therapeutic work.
The "Pure-O" has two parts: the originating unwanted thought (spike), and the mental activity in which the sufferer attempts to escape, solve, or undo the spike. This is called “rumination.” With “Pure-O”, it is the threatening, nagging, or haunting nature of the idea, which compels the patient to engage in an extensive effort to escape from the thought. Most likely, it is not the intrusive idea, per se, that drives the response, but the associated emotional terror. The following are some illustrations of these types of “Pure-O” situations.
1. A man is involved in sexual relations with his female lover. Just prior to orgasm, the thought of his friend Bob pops into his head. This is the fourth time in a month that this has happened. In response to this, he becomes very upset and wonders whether or not he is gay. His sexual activity is terminated in order to avoid having to deal with this concern.
2. A mother is changing the diaper of her infant. As she lovingly looks down at this helpless child, the thought occurs to her to "take a pillow and smother him." In response to this thought, the mother panics and runs to another room to diminish the possibility of acting on this thought, because she feels that having the thought is tantamount to acting on it.
3. A student finishes a conversation with his favorite professor. For the next three hours the student reviews the conversation mentally to ascertain if he said anything that might have been offensive.
4. An altar boy in church notices a statue of the Virgin Mary. He has a fleeting thought passes about performing a sexual act on her. He is tormented endlessly, even though he has repeatedly confessed the thought to a priest and to his parents.
5. A young man notices that the word “suicide” possesses a significant repugnance. It is not that he is depressed; he feels that the word suicide “shouldn’t” stand out. He finds that, not only does encountering the word in print produce a tremendous amount of emotional tumult, but hearing it in his own thoughts becomes equally upsetting. Certain sounds also start to stand out as being unique and unsettling. He begins to spend a great deal of time wrapped up in his own thoughts attempting to arrange the word in a certain manner so that it possesses less significance. He becomes tormented by the possibility that the unique sounds surrounding him may linger on for eternity and determines that he must find some method to stop being reminded of their occurrence.
6. A woman survives emotional abuse from an overly controlling father. At 20, she leaves his house, and she’s elated. However, she develops an obsession. She decides that all objects, which remind her of him, are infused with his essence and, therefore, must be discarded. Although irrational, she feels that discarding anything related to him will keep her identity free from his influence. She feels that to completely free herself from him, she has to discard all objects that remind her of her father, even those that might have been “contaminated” by contact with his possessions. This effort to free herself from her father’s influence, becomes so encompassing that she has to avoid even mail from her siblings because her father might have come in contact with something that had come in contact with the mail.
For the person suffering with the "Pure-O", a tremendous amount of anxiety and/or guilt accompanies the spike. The mental ritual (rumination) is the volitional effort to shut off the anxiety, either by attempting to gain reassurance, solve the question, or avoid having the thought recur. The tormenting thought (spike) typically entails two parts. The first is the idea that the thought, in and of itself, is deviant and signifies something horrible about the person who has it. “I must be a sick, mentally unstable person to have had this thought occur.” Or, “Only a ‘bad’ person could think such a thing.” The second part is the great emotional and physical discomfort accompanying the intrusive idea. The symptoms of anxiety can include, but are not limited to: rapid and heavy heartbeat, upset stomach, excessive perspiration, muscle fatigue, mental thoughts and/or muscular tension. These symptoms are what make people with OCD “feel” that the spike is so problematic. It is during the rumination phase that the person's mind becomes extremely preoccupied and distracted. It is not unusual for someone with the “Pure-O” to spend endless hours trying to “escape” from these thoughts. The perceived need to stop these thoughts is tremendous. A common misconception among “Pure-O” sufferers is that there is a way to turn off the obsession, and that they just have to keep obsessing until they hit upon that way. If they can find “the answer,” the right thought, then the obsessing will just vanish completely. Most sufferers realize this is an impossibility, but they cannot give up the search.
The accompanying diagram illustrates the endless cycle of spiking and ruminating. On the left-hand side of the diagram you will see references to “subconscious mental processes” and the “anxiety center." The subconscious mental processes are located in the outer portion of the brain and represent parts of the brain that are creative and always on the lookout for pertinent information. Evidence of its existence lies in a phenomenon known as the "Tip-of-the-Tongue" effect (Brown & McNeil, 1966). All of us have had the experience of searching for a word or fact that is just on the tip of our tongue, but continues to elude us. So we give up trying to recall it and go about our business. Then, later, it pops into our consciousness, even though our mind is preoccupied with another topic. I believe that there is a non-conscious portion of the brain that searches our meaningful material and sends this information to one’s consciousness. One tends to more readily notice information that has a strong association component with significant material than non-relevant information. For example, when we see a red light, we immediately react to it as a warning (i.e., unconsciously, we associate a red light with the idea of a hazard). For the "Pure-O" sufferer plagued with thoughts of violence, the sight of a knife might spike the thought of stabbing a loved one. The “Anxiety Center” (left side of the diagram) is closely associated with the “Subconscious Mental Processes” (see diagram). This part of the brain is called the amygdala. Brain mapping studies suggest that the amygdala is active when we experience emotional upheaval. On occasion, the amygdala is triggered by an external stimulus, e.g., finding a snake in one’s camping tent. In the case of panic attacks, seemingly random events can trigger the amygdala to misfire and send the same types of signals. The Anxiety Center is responsible for the fight-or-flight response. Brain mapping studies suggest that the amygdala is the center of visceral awareness that there is an urgent threat demanding immediate attention. The Anxiety Center activates psychological responses to emotional information, such as, rapid heart rate, racing thoughts or upset stomach. The resource center transmits information to our conscious awareness that deems material relevant or significant. It is at this juncture that most “Pure-O‘s” becomes fixated and distraught.
The transmission of the information from these subconscious processes to our conscious awareness is a purely reflexive one and beyond our control. However, it is not beyond our influence. When the spike reaches our “conscious awareness", we have a choice as to how to process the thought (represented by the two arrows in the attached diagram). The arrow pointing upward suggests that the person experiencing the stimulus chooses to believe that the spike thought represents or reflects something deep and meaningful about the person; e.g., "only a vicious, loathsome human being could possibly think of stabbing their loved one." This is referred to as the “instinctive response” (IR) because it is inherent within each person to resist anything which feels so threatening. People with OCD are not less tolerant of these upsetting ideas, which most humans report are a natural part of their daily existence. It is just that people with OCD experience a “misfire” in the brain, which makes them “feel” as if the idea is problematic. Usually, an effort is made to seek reassurance and disqualify the legitimacy of these upsetting ideas and threatening experiences.
The instinctive responses naturally produce the strong desire to engage in resistance and relief seeking. This represents, as Albert Ellis (1987, 1991) has suggested, a dysfunctional emotional response. The tremendous effort one puts into escaping the unwanted thoughts or preventing their recurrence (e.g. hiding knives), in effect reinforces (e.g. strengthens the association) its importance to the non-conscious brain and thereby feeds the vicious cycle. This process is represented in the accompanying diagram by the arrow pointing from the top box back toward the anxiety center. Similar notions have been proposed by Wenzlaff, Wegner, & Roper (1988). These authors suggest that attempting to suppress thoughts has the effect of making them stronger. Recognizing that you are upset by a thought and then reacting with resistance places a mental marker on it and, therefore, increases the likelihood of the thought reoccurring. For the sufferer with "Pure-O," the spike is a double barrel shot of anxiety. First, there is anxiety for having such an unpleasant or deviant thought. Then, the tremendous, uncontrollable repetitiousness of the thoughts makes the sufferer think he is losing his mind. The uncertainty regarding mental loss of control can be a very anxiety provoking experience.
As per the “Conscious Awareness” box in the diagram, the arrows pointing downward represent the least likely response, but, ultimately, the most therapeutic one. The extinction response entails recognizing the existence of the “bad” thought, but assigns no blame to the person for having it. This response allows the upsetting ideas to exist, despite the presence of the accompanying extreme anxiety. Many cognitive-behavioral psychologists believe that the absence of this response is what distinguishes people with OCD from the “normal” population. In contrast, the cognitive psychologist believes that just by shedding light on either the irrationality of the idea of being a bad person or on the person not being responsible for the initiation of the thought, relief from anxiety will result. However, those with OCD might suggest that, in order for psychologists to fully understand what they experience, their amygdalas could be stimulated to the point of feeling like the world is ending. The experience of feeling compelled to then “run for the hills” would be shared. The extinction response is not the reflexive one, nor does it occur naturally when feeling so unsettled. In fact, the extinction response feels so unnatural because it is diametrically opposed to what we are evolutionarily wired to do when faced with anxiety. Therefore it is crucial for the patient to understand that OCD involves faulty wiring, not an irrational belief system.
For a behavioral psychologist, the key issue is not how or why these thoughts become out of control, but what to do about them when they're racing around in one's head eight hours a day. It is extremely distressing that this form of OCD continues to present such confusion for mental health professionals. There remains a good deal of ignorance regarding appropriate treatment strategies and conceptualizations. Today the most common trend for cognitive-behavioral psychologists is the use of “rational responding” as a means of managing Pure-O. Although people with OCD “feel” as if the obsessive thought is legitimate, they typically remain steadfastly aware that they are performing extensive or elaborate escape responses for no logical reason. Clearly, it does not make sense that the therapeutic objective should be to help the patient “find the evidence” that the thought is illegitimate.
But before discussing what works, first it is critical to discuss what does not work!
Thought stopping, both through shouting, “STOP” or snapping a rubber band in response to the spike, is clearly not recommended and may actually be detrimental. As discussed previously, this technique sensitizes the brain to the unwanted thought by alerting the anxiety center that potential punishment is associated with the spike. Theoretically, the spikes would thus increase due to this heightened sensitivity. Research to date has demonstrated that these techniques are not effective treatments of OCD.
Although logically pointing out the absurdity of the "pure-O" patient’s mental rituals is very tempting, it is often insulting and clearly ineffective. You cannot "outlogic" OCD. People with OCD are understandably drawn to this type of therapy because the therapist is actually reassuring the patient by helping the desperately anxious patient see the irrational nature of these threatening ideas. This type of treatment ultimately can make the patient dependent on the therapist’s determinations of what is rational and what is not, and is therefore an ineffective treatment approach.
Another treatment approach involves the use of analytic interpretations. This approach assigns meaning and significance to the content of the spike and attempts to instruct the patient to “understand” this meaning. This understanding or insight supposedly is both necessary and sufficient to produce change. However, we now believe that this approach for OCD is not only ineffective, but actually is detrimental and may further fuel and reinforce the OCD process. Nevertheless, many people with untreated Pure-O are unfortunately still drawn to this type of therapy approach, as they have a natural inclination to investigate, make meaning of their spikes, and find solutions to their upsetting thoughts. The process of trying to find solutions to alleviate the anxiety and upset is referred to as rumination, and is clearly part of the maladaptive management of the disorder. Initially, when an OCD patient begins behavior therapy after years of analytic or insight therapy, he needs to be deprogrammed. Only then can the full benefit of behavior therapy be achieved.
In 2004, while there is a great deal of scientific evidence that thought stopping, rubber band therapy, and analytical therapy are not recommended and are ineffective for treating OCD, many psychologists are debating whether or not there is any benefit to using cognitive strategies as an additional component to behavior therapy. The idea behind fundamental behaviorism is to change brain chemistry through conditioning. The underlying belief is that patients with anxiety disorders do not have defects in their thinking processes. In a well-known study done by Freeston, et al. (1997), the treatment consisted of cognitive strategies as well as traditional behavioral strategies. The combining of therapies makes it difficult to know whether the cognitive approach added to or detracted from the patients’ recoveries.
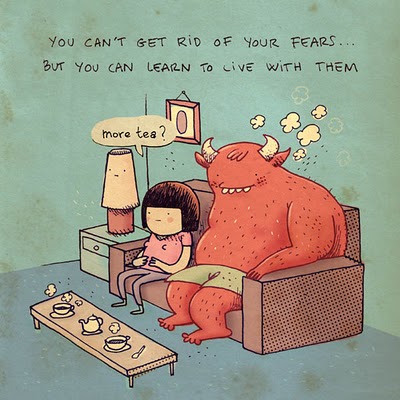
Ultimately, as with all forms of OCD, learning to live with uncertainty and risk-taking are the antidotes to this disorder. The treatment of the "Pure-O" is theoretically based on the principles of classical conditioning and extinction. The disorder is perpetuated by the patient’s need to try to rationalize and control any random, bizarre, and noxious thoughts that occur to him. This intolerance exists due to a misfiring brain function, which makes the patient feel that the thought itself is equal to acting on such a thought. The efforts a person makes to avoid or escape these thoughts reinforce their reoccurrence
It is given that a patient’s spike will increase when he begins using ERP. The human is resistant to change. Commonly a person who, before treatment, would spoke many times per day and then ruminate incessantly for the duration of the day, will, after behavior therapy, spike much more frequently, but ruminate much less. The goal of this therapy is not to make the thought go away or to achieve anxiety relief. Although this statement sounds peculiar, it should be repeated often and emphasized during the initial stages of therapy. Rather, the goal of this therapy is to provide specific guidelines for effectively managing this condition so that the brain can naturally readjust to a non-reactive state.
The critical point to be made is that eliminating rumination is the goal, not eliminating the number of spikes! It’s how we manage challenges that determines the quality of our lives. The goal of therapy is to not respond to the spike. The goal is not to eliminate the existence of the spikes. Interestingly, though, the long-term effect of not attending to the spike will be that the spikes in fact will decrease in frequency and emotional intensity. However, this will happen only if the person becomes desensitized to these thoughts by allowing them to occur. A common phrase often mentioned in cognitive-behavioral groups that I run is "Let the thoughts be there, Give yourself permission to have the thoughts.” A patient has to learn to be able to manage that the occurrence of any thought, no matter how bizarre or horrific, has no meaning.
The following useful suggestions are offered towards managing obsessions.
The research is still preliminary, but the treatment outcomes have been significant enough to spread the word. As with all forms of OCD, behavioral therapy is effective to the extent that the patient adheres to the procedures (Dar & Greist, 1992). Since this article’s original version, two procedures (index card therapy and spike hunts) have been added to the therapeutic arsenal and have been proven effective. I am just outlining these procedures because behavior therapy needs to be done with an experienced practitioner. Attempting to implement these techniques without expert guidance can be problematic and prevent goal attainment.
1. The Antidote Procedure
The spike often presents itself either as a question or potential disastrous scenario. A response, which answers the spike in a way that leaves ambiguity, is the antidote to preventing rumination. For instance, if the patient has the thought "If I don't remember what I had for breakfast yesterday my mother will die of cancer!" Under the Antidote Procedure, to manage the obsession, the most therapeutic response a patient can have is to accept this possibility and be willing to take the risk of his mother dying cancer or the question reoccurring for eternity. There is often a question regarding the degree to which one “really needs to believe” that their mother might die. In response, it is important to understand that ones’ beliefs are really not a significant component of treatment success. Instead, the behaviors and choices one engages in are key to conveying to one’s brain that the theme is no longer going to be any importance The goal is to expend the least amount of effort is responding to the question. In another example, a spike might be, "Maybe I said something offensive to my boss yesterday." A recommended response would be, "Maybe I did. I'll live with the possibility and take the risk he'll fire me tomorrow." Using this procedure, it is imperative that the distinction be made between the therapeutic response and rumination. The therapeutic response does not answer the question posed by a spike.
2. Let It Be There:
Using this procedure, it is suggested that the person create a mental pigeon hole for the disturbing thoughts and accept the presence of the thoughts into one's preconscious (those thoughts which are not currently in one's awareness but can easily be brought there by turning one's attention to them, i.e. your name or phone number). It is suggested that a mental "hotel" be created whereby you encourage your brain to store all the unsolvable questions so as to fill up the register. The more unsolved questions the better. It is critical that the person suffering from the “Pure-O” acknowledge the presence of these thoughts, but pay no further attention to them by trying to solve the problems presented by them. The brain can only juggle a certain amount of information at one time. If you purposely overload the brain, rather than going insane, your brain’s response will be to just give up trying. A key to this technique is that the person trying it has to have a great deal of faith and trust in the therapist suggesting it.
3. Spike Hunt
Very similar to the “let it be there” approach is the spike hunt. Using this procedure the patient is encouraged to purposely seek out spikes. This process actually is a 180-degree reversal of the reflexive OCD momentum. Most people’s OCD desperately hope for the associations to go away and never return. This frame of mind actually increases the susceptibility of the mind to these thoughts and exacerbates the condition.
A good example of a spike hunt is:
Patient X is terrified that he might get up in the middle of the night and violently assault his wife and child. He is so fearful that he might act on these thoughts, that any bump or strange shadow in the bedroom prompts him to consider that it might be a place where he’s hidden a knife or a gun with which to harm his family. Even familiar objects, which are out-of-place, seem to suggest that he is capable of acting in a non-conscious way and thereby lend support to the idea that his family is in danger of his uncontrollable/non-conscious actions. Using the spike hunt, this patient was instructed to purposely find unidentifiable shadows or mysteriously placed objects and gather together evidence that the world of the unknown lurks out there and represents possible unforeseen peril. After using this technique for two months and sleeping next to a steak knife, the patient achieved approximately 75% symptom relief. The rationale for this seemingly contradictory approach lies in the behavioral principles of reconditioning. Reconditioning retrains the brain to consider its warnings to be non-relevant. For human brains non-relevant information equals experiences that are not perceived.
4. The Capsule Technique
During the initial phases of therapy, there is a great resistance to letting go of the rumination. A procedure to handle this resistance is to have the person with OCD to set aside a specified period of time, perhaps once or twice a day, to purposefully ruminate. It is suggested that the time periods be predetermined and time limited. The patient should tell himself “At exactly 8:15 a.m. and 8:15 p.m. I will ruminate for exactly 45 minutes. As thoughts occur to me other times during the day, I can feel comforted that the problem solving will be given sufficient time later that evening or early the next morning.” Typically, people report that it is difficult to fill the allotted rumination time. Regardless, every minute must be spent on the designated topic so the brain can habituate to these irrelevant thoughts. A novel application of this technique was reported in the Journal of Behavior Therapy and Experimental Psychiatry. Using audiotaped spiking material a woman was desensitized to her obsessional themes by exposing herself to them ten times a day. After the fiftieth day, her actual spiking dramatically decreased.
5. Turning Up the Volume
Rather than attempting to escape the spikes, the person with "Pure-O" is encouraged to purposely create the thought, repeatedly, following its initial occurrence. One is also encouraged to take the presented topic and actually amplify the threatening component. This has the effect of desensitizing the brain to these spikes by sending the message that not only am I not going to attempt to escape these thoughts; but I am at such peace with them I can create a multitude of them. In response to the thought, "I might have run over someone on my way to work," a beneficial response would be; "There is probably a stack of bodies all along the street; I probably wiped out half the population of my home town yesterday as well. I can't wait to drive home tonight and kill the other half."
6. Index Card Therapy
The index card therapy procedure has been an extremely useful in treating people with “Pure-O.” What baffled behaviorists for years in attempting to treat this form of OCD was that there was no object with which the patient could actually perform an exposure exercise. It seemed rather difficult to have a person touch the thought “Kill my baby” or “I hate God” and then spread it all over the place. To concretize these thoughts Dr. Foa has suggested using loop tapes in which a patient would sit and listen to his/her their particular obsession played over and over ad-nausea. The possible limitation of this procedure is that the patient might become habituated to the voice on the tape and not the actual theme represented on the tape. In addition, carrying a tape recorder around with you might be cumbersome and most people do not have an hour each day to sit and just listen to the same message played over and over again. So to remedy these problems I created index card therapy, where the patient writes the topic of the spike down on an index card. The patient would also record the date, the intensity of the spike, and the level of resistance to the spike on the index card. The writer carries the index card with him at all times, preferably in a pocket. The patient periodically reviews the index card or cards, usually about six to ten times per day, until the level of associated anxiety and resistance is below a rating of two out of ten for two consecutive days.
Some people report that they have difficulty distinguishing between spikes and "legitimate important thoughts." A foolproof litmus test for telling the difference is to ask yourself, “Did the thought or question come with an associated anxiety, feeling of urgency or feelings of guilt?” Ultimately it is wise to place such thoughts in the realm of OCD and make the CHOICE to accept the risk. When asked, "What if it's not OCD," I say "Take the risk and live with the uncertainty." For those who have made significant progress in the Pure-O process, a common complication involves distinguishing a therapeutic response from a ritual.
The “Exposure and Response Prevention paradigm seems simple. If it makes you anxious, confront it! Create a hierarchy and gradually work your way toward the most challenging items. At some point most Purely Obsessional patients almost always come up with the same question: “Am I doing the therapy correctly?” It is very common obsessional reaction to someone doing behavior therapy. The mind tries to throw a monkey wrench into the therapeutic machine by asking the question, “Which is the actual therapeutic response: the performance of an exposure exercise or just accepting the risk?” The ensuing effort to secure the correct answer to this question ultimately can, unchecked, become a time-consuming ritual itself.
To illustrate this dilemma, let’s look at the naturally occurring behaviors of blinking and swallowing. For instance, the mind tells the patient to swallow or blink, now! The dilemma is as follows: “If I swallow now, won’t that be giving into the spike? If I resist giving into the command, then I’m avoiding engaging in the naturally occurring action of swallowing. What’s a good patient to do?” The very skilled patient will now accept that all blinks in the future will be the “wrong” blink and accept that all blinks are actually performing a ritual. This choice will influence the brain to stop scrutinizing “getting the therapy right.” Ultimately most Pure-O’s and people with a perfectionistic mentality end up spending a great deal of wasted time making sure that they are managing the disorder in a “correct” way. Living in a world of no answers is essential to being able to make a choice and move on.
At this point, the skills of any therapist are not nearly as valuable as the client's willingness to utilize the procedures. Unless a sufferer is thoroughly fed up with the disorder, behavior therapy will be of limited help. Often I have been informed that the treatment is as painful as the disorder. My only response is that with this treatment there is a light at the end of the tunnel. The disorder offers only endless suffering. If you find that after six months to a year there is limited movement in a positive direction, it might be worth your while to take a temporary leave of absence from therapy until you are fully committed to letting go of the problem. Published clinical notations suggest that this step might assist in bringing about an increased willingness to confront the nightmare rather than to continue to mentally run away from it.
------------------------------------------------------------------------
References
References for the Article are available by emailing perkins@ocfoundation.org
Tags: CBT, Cognitive Behavioral Therapy, OCD, Obesessive Compulsive Disorder, Pure O., Perfectionism, Perfectionist